Near the end of World War One, a nasty flu started spreading around the world. The virus responsible for the disease, which became known as Spanish flu, infected over a quarter of the world’s population. With an estimated death toll of between 50 million and 100 million, it was one of the deadliest pandemics in human history.
In the midst of this pandemic, during September 1918, cities around the US were planning parades to promote liberty bonds, being sold to help pay for the war effort in Europe. In Philadelphia, Pennsylvania, where 600 soldiers were already infected with the flu virus, city chiefs decided to go ahead with their parade. Meanwhile, the city of Saint Louis, Missouri, opted to cancel their parade and introduce other measures to limit public gatherings. One month later, more than 10,000 people in Philadelphia had died of Spanish flu, while the number of fatalities in Saint Louis stayed below 700.
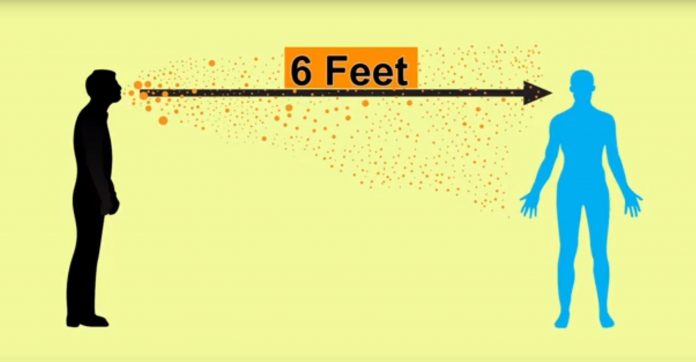
The parade was not the only reason for the difference in death rates, but the figures show the importance of measures now known as “social distancing” can have during pandemics. “Social distancing refers to a way of creating a barrier of physical distance between two or more people so that transmission of virus can be prevented or halted,” says Arindam Basu, associate professor of epidemiology and environmental health at the University of Canterbury, in New Zealand.
One analysis of the interventions made in several cities around the US during 1918 showed that those that banned public gatherings, closed theatres, schools and churches early had far lower peak death rates.
Just over 100 years later, the world is facing another pandemic, this time from a different virus – the Covid-19 coronavirus. Today the global population stands six billion higher than it did in 1918. While Covid-19 is different in many ways from the Spanish flu – particularly in terms of who it affects and its mortality rate so far – there is a very important lesson about the difference social distancing can make. It might still be one of the best ways of fighting this pandemic. (Read more about the other lessons we can learn from Spanish flu.)
The death rates in Philadelphia and St Louis during the 1918 Spanish flu pandemic demonstrate the importance of social distancing (Credit: National Academy of Sciences USA 2007)
“At this time, we do not know of a safe and effective vaccine, nor do we know if a safe and effective drug will work to eliminate the Covid-19 infection once it has occurred,” says Basu. “In the absence of these, our best bet is based on prevention.”
Many countries around the world are now experiencing different measures in an attempt to enforce social distancing to slow the spread of Covid-19. They range from ending mass gatherings, closing public spaces like leisure centres, pubs and clubs to closing schools and in some places a total lockdown with people forced to stay indoors.
While self-isolation is a form of social distancing, there is an important distinction to be made. Self-isolation and quarantine are aimed at preventing people who are infected or are known to have had contact with people who are infected from passing on the virus. Social distancing is a wider measure aimed at stopping the kind of mixing of people that allows infections to spread through a population.
Each person infected with the Covid-19 coronavirus is thought to pass it on to an average of 2-3 other people in the early stages of an outbreak. This contagiousness is measured by epidemiologists using something known as a “reproduction number”. By comparison, influenza has a reproduction number of 1.06-3.4 depending on the strain. Spanish flu was found to have a reproduction number of about 1.8 by one study. Rhinovirus, which is one of those that causes the common cold, has a reproduction number of 1.2-1.83. Most estimates for Covid-19 have put its reproduction number at between 1.4-3.9.
What exactly is social distancing?
The incubation period – the time between infection and symptoms appearing – has been found to be around five days for Covid-19, although it can take up to 14 days for symptoms to appear, according to research in China. If you are infected, and continue to socialise as normal, it is likely you will pass the virus on to between two and three friends or family members, who could each then go on to infect a further 2-3 people. Within one month one case can lead to 244 other cases in this way and in two months, this soars to 59,604.
See Also: Fight against illicit trade of petroleum products yields dividends
To further complicate this, the virus is also thought to be able to spread from people who have been infected but yet to show any symptoms. One study by Lauren Ancel Meyers at the University of Texas at Austin estimated that this silent transmission can occur in up to 10% of cases. An estimated 1-3% of people who catch the disease will remain asymptomatic. These people might not know to self-isolate, but if they observed good social-distancing practices would be prevented from spreading the virus unwittingly.
There is already some evidence that staying at home, and maintaining a safe distance from others, can slow the spread and stop this domino effect. Research looking at infections in Wuhan showed that the introduction of large-scale control measures saw the reproduction number in the city fall from 2.35 to almost one. When a reproduction number reaches one, the number of cases will stop rising as effectively each infected person is passing it on to just one other person.
Modelling work in China has shown that substantial levels of social distancing was key to reducing this reproduction number in Wuhan and the wider Hubei region. It concluded that the earlier a lockdown is put in place in the epicentre of an outbreak, the smaller it ends up being.
The time between infection and symptoms appearing has been found to be around five days for Covid-19
One of the main aims of social distancing is to “flatten the curve”, which means delaying the spread of the virus so it reaches people more slowly. The idea is to lengthen the time period over which the virus travels through a population and push the peak number of cases back so it appears later. A graph showing the number of infections would peak much more quickly without social distancing. With it, the curve is much flatter, meaning at any given time the number of infected people, and therefore people needing urgent care and resources, is lower.
But how does this translate to real life situations? Different countries have taken different approaches to prevention strategies. The UK is among those that has been stepping up its efforts in response to a report using computer modelling to predict how the virus might spread by researchers at Imperial College London, published on 16 March.
The scientists looked into two potential methods of tackling the pandemic in simulations of the UK and the US populations. The first, mitigation, focused on only socially isolating those most at risk and quarantining those with symptoms. The second, suppression, involved everyone in the population taking steps to social distance themselves while those with symptoms and others in the household quarantine themselves at home.
Countries around the world are implementing measures to encourage social distancing (Credit: Getty Images)
The paper found that without any measures at all the UK could face 510,000 deaths while the US could expect 2.2 million from Covid-19. While they estimated the first mitigation strategy could potentially reduce demand for healthcare by two thirds and halve the number of deaths, it would still result in hundreds of thousands of people dying. It would also still overwhelm the health services, particularly intensive care, “several times over”.
Before the report was published, the UK was aiming to achieve “herd immunity”, a situation in which a substantial proportion of the members of a society become immune, either following an infection or by vaccination. By shrinking the pool of people who can catch the infection, this herd immunity effectively halts the virus from spreading much further.
“When herd immunity is used as a strategy, those who use this allow some practices, knowing well that it can potentially spread infection,” says Basu. “Things such as mass gathering are still allowed with a view that people who will attend them are healthier and ‘stouter’ and will recover and in the process confer immunity to others.”
When it comes to Covid-19, Basu says, we know very little about the short- and longer-term consequences of infections. It is also still not clear how much immunity people who have been infected develop once they recover (although sometests in monkeys suggest it is possible to develop immunity following infection)..
“So knowingly exposing otherwise healthy individuals and letting an infection spread through when isolation or lockdown may work can be dangerous,” says Basu. “If people who are infected pass infection to other susceptible people who live with them, then the situation can escalate very quickly.”
In response to the Imperial research, the UK government changed its advice, introducing increasingly strict control measures and restrictions on businesses and the public.
The age of a population, as well as the way people live in a society, has a big impact on how Covid-19 is spreading, according to researchers at Oxford University and Nuffield College.
Jennifer Dowd and her colleagues looked at the demographics and spread of the disease in different parts of the world. In Italy, which has an older population and intergenerational families tend to live more closely together, the Covid-19 virus has claimed more lives. This is because the fatality rate in people over 80 is estimated at 14.8%, compared to 0.4% for those aged between 40 and 49, according to their study of cases and deaths up to 13 March.
But even in Italy, social distancing seems to have had an impact. Different strategies implemented in two towns – Bergamo and Lodi – have led to a striking difference in the number of infections.
In Lodi, the first case of coronavirus was detected on 21 February, and travel restrictions were implemented two days later. “On 24 February, all schools, universities, cultural, recreational and sporting events were also cancelled,” says Dowd. “Cases also began to be discovered in Bergamo on 23 February within a small number of municipalities, and there was press discussion of similar restrictions, but this was not enacted until the broader shutdown on 8 March.”
On 7 March, both towns had around 800 cases, but by 13 March Bergamo’s number of cases had risen to around 2,300 while Lodi’s had just under half that amount at around 1,100. The two provinces have similar age structures, both with roughly 21% of the population above age 65, says Dowd.
“While Bergamo overall has a larger population than Lodi, the clusters of municipalities in which cases originated were of similar size and thus comparable for looking at the early progression of the outbreak,” says Dowd.
The situations look astonishingly similar to those seen in Philadelphia and Saint Louis. But it is still too early to say if history will repeat itself, the researchers say. One major difference is the numbers they are comparing in these Italian towns are cases of the virus rather than deaths.
The Italian town of Lodi put social distancing measures in place much earlier than Bergamo, where cases rose more sharply (Credit: Leverhulme Centre for Demographic Science)
“There could be other things that differed across these contexts such as particular super-spreading event, different social networks,” says Dowd. “But given the similarity at baseline and the extreme interventions that happened in Lodi, we think it is strongly suggestive of the effectiveness of these measures.”
Overall, says Dowd, it is safe to say social distancing works. “We are seeing real evidence for the effectiveness of these measures.”
Overall, says Dowd, it is safe to say social distancing works. “We are seeing real evidence for the effectiveness of these measures.”
Another study in Washington State that looked at the spread of respiratory viruses in general – but not Covid-19 – showed that social distancing can reduce the spread of these diseases over the long term too. Unusually high snowfall in February 2019 led to widespread school and workplace closures, which saw a reduction in cases over the rest of the season of 3-9%.
Of course, staying away from friends and family is not easy, especially during a global pandemic. There can be some unintended consequences that come from avoiding people. In the long term, staying isolated from social groups is linked to heart disease, depression, and dementia.
But social distancing does not necessarily mean stopping all contact. Unlike in 1918, today there are plenty of ways for people to stay in touch with loved ones. Technology has brought us social media, messaging apps and online video calls.
And if it keeps the ones we love around us safe, it may ultimately be worth it.
thebftonline


























